For many people with temporomandibular joint (TMJ) discomfort or dysfunction, traditional treatments like oral splints, physical therapy, or pain medications may provide only limited relief. In that context, TMJ Botox before and after results have gained attention as a treatment option aimed at reducing muscle tension, easing pain, and improving jaw mobility. But what can you realistically expect from this treatment, how does it work, and is it right for you? In this comprehensive guide, we explore everything from how Botox helps relax muscles to the typical timeline of results, potential risks, and real-world considerations so you can make informed decisions about your TMJ care.
Table of Contents
- What Is TMJ Botox?
- How Botox Works for TMJ Disorders
- Expected Results: TMJ Botox Before and After
- Who Might Benefit Most
- Procedure, Timeline & Recovery
- Risks and Side Effects
- Alternatives and Complementary Therapies
- When to Talk to a TMJ Specialist
- FAQs
- Final Thoughts
1. What Is TMJ Botox?
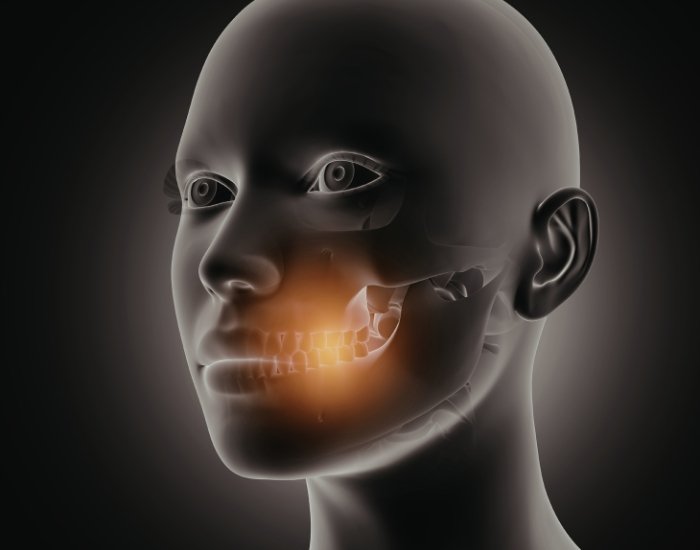
TMJ Botox refers to injections of botulinum toxin into specific jaw muscles that are overactive or tense in individuals with TMJ disorders. The toxin temporarily blocks nerve signals that tell muscles to contract, which leads to muscle relaxation and reduced force during activities like chewing or clenching. The treatment is not FDA-approved specifically for TMJ disorders, meaning it’s often used “off-label” after more conservative therapies have been tried first.
Unlike cosmetic Botox, which is aimed at reducing wrinkles, TMJ Botox targets the masseter, temporalis, and other jaw-related muscles to reduce hyperactivity that can contribute to pain and dysfunction.
2. How Botox Works for TMJ Disorders
When injected into jaw muscles, botulinum toxin interrupts communication between nerves and muscles. This causes the muscle fibers to relax and contract less forcefully. With reduced contraction, muscle tension decreases, which can ease pain, prevent grinding, and help break the cycle of dysfunction that commonly contributes to TMJ pain and tightness.
This muscle-relaxing effect typically begins within a few days of treatment and reaches its peak around 10 to 14 days. The impact is temporary, meaning follow-up sessions may be needed every three to four months to maintain symptom relief.
3. Expected Results: TMJ Botox Before and After
When considering TMJ Botox before and after outcomes, it’s important to set realistic expectations. Many individuals report:
- Reduction in jaw tension and clenching, leading to less pain during eating or speaking.
- Decreased frequency and intensity of headaches associated with jaw muscle overactivity.
- Improved ease of jaw movement and reduced muscle stiffness.
- Smoother jaw function, with less popping, grinding, or locking.
- Changes in facial muscle bulk over time, which may appear as a slightly softer jawline for some people.
These results are generally more noticeable within two weeks after treatment and can last three to five months. Follow-up treatments are common for sustained relief.
It’s worth noting that Botox does not cure underlying structural issues within the TMJ, such as disc displacement or arthritis, but it may improve symptoms when muscle hyperactivity plays a significant role.
4. Who Might Benefit Most
Botox therapy is most often considered for patients who:
- Have persistent jaw pain or tightness that resists conservative care like oral appliances, physical therapy, or medication.
- Experience frequent teeth grinding (bruxism) or clenching at night.
- Notice frequent headaches that radiate from jaw tension.
- Have difficulty relaxing jaw muscles despite daily exercises.
Remember, Botox tends to address muscle tension and activity, so it’s typically more helpful when muscle overactivity contributes significantly to symptoms. For conditions rooted primarily in joint degeneration or structural issues, other treatments may be more effective.
5. Procedure, Timeline & Recovery
A TMJ Botox session is typically quick and performed in an outpatient setting. The provider injects small, controlled amounts of Botox into targeted jaw muscles that are contributing to excessive tension or overactivity. These muscles are often involved in broader TMJ Dysfunction, where abnormal muscle function places stress on the temporomandibular joint and surrounding structures. The procedure usually takes less than 30 minutes and does not require anesthesia, though a topical numbing agent may be used for comfort.
After treatment, most patients are able to resume normal daily activities the same day. Mild soreness, tenderness, or swelling at the injection sites can occur but typically resolves within a short time. Muscle relaxation generally begins within a few days, with more noticeable improvement developing over one to two weeks. As muscle activity gradually returns over several months, follow-up treatments may be considered based on symptom response and individual needs.
6. Risks and Side Effects
As with any medical treatment, TMJ Botox carries potential risks and side effects, though many are temporary and mild. Common effects include localized tenderness, bruising, or swelling at the injection sites. Some individuals may notice temporary muscle weakness, which can affect chewing strength for a short period. These effects usually resolve as the Botox wears off.
Less commonly, unintended spread of the toxin may lead to temporary changes in facial movement or expression. Because TMJ Botox targets muscle activity rather than joint structure, it is important to understand how it fits within the broader picture of tmj symptoms, which may include jaw pain, clicking, stiffness, headaches, or ear discomfort. Botox may help reduce muscle-related symptoms, but it does not correct underlying joint damage or disc displacement.
A thorough evaluation by an experienced provider helps determine whether the potential benefits outweigh the risks and whether Botox is appropriate as part of a comprehensive TMJ treatment plan.
7. Alternatives and Complementary Therapies
Botox is one option among many for managing TMJ-related pain and dysfunction. Other approaches may include:
- Physical therapy and jaw-focused exercises
- Oral appliances or splints
- Stress management techniques
- Anti-inflammatory medications
- Lifestyle changes such as posture correction and avoiding hard chewing
Some patients may find greater benefit when Botox is used alongside these therapies rather than as a standalone solution.
It’s also worth exploring the broader context of your symptoms — for example, the relationship between TMJ discomfort and other conditions like TMJ Pain on One Side or TMJ Nerve Damage Symptoms — as well as understanding how the joint functions and can be affected overall through concepts discussed in TMJ Dysfunction and TMJ symptoms resources.
8. When to Talk to a TMJ Specialist
Botox may be most appropriate for people whose symptoms haven’t responded to initial, less invasive treatments. You should consider consulting a TMJ specialist if:
- Pain, tension, or clicking continues despite self-care and therapy.
- Symptoms interfere with eating, speaking, or quality of life.
- You experience frequent headaches or referred pain related to jaw tension.
- You’re curious whether Botox might be an option for your specific TMJ symptoms.
An experienced clinician can help determine whether Botox aligns with your treatment goals and tailor an approach suited to your needs.
9. FAQs
Q1: How long do TMJ Botox results last?
A: Relief typically lasts about three to five months, after which movement and tension gradually return.
Q2: Is Botox a cure for TMJ disorders?
A: No. Botox eases muscle tension and related symptoms but does not solve structural joint issues.
Q3: Does TMJ Botox help reduce headaches?
A: Many patients report fewer tension-related headaches following treatment due to reduced muscle overactivity.
Q4: Is Botox for TMJ painful?
A: Most people report mild discomfort similar to a quick pinch, and the area may feel tender afterward.
Q5: Can anyone get TMJ Botox?
A: Botox isn’t appropriate for everyone; your doctor will assess health history, symptoms, and goals before recommending it.
10. Final Thoughts
TMJ Botox before and after results vary from person to person, but many individuals find meaningful relief from muscle tension, pain, and related symptoms when conservative treatments alone aren’t sufficient. Understanding how Botox works, what it can realistically achieve, and the associated risks empowers you to make informed decisions about your TMJ care. Whether Botox becomes part of your treatment plan or you explore alternative therapies, working with a qualified provider ensures the safest and most effective approach for your unique condition.
If you’re curious about whether TMJ Botox before and after results might apply to your situation, reach out to Relief TMJ today. Their experienced team can help assess your symptoms, discuss individualized treatment options, and support you on your pathway to comfort and better jaw function.
Medical Disclaimer: This blog is for informational purposes only and does not replace professional medical advice, diagnosis, or treatment. Always consult a qualified healthcare provider with questions about your health or treatment options.